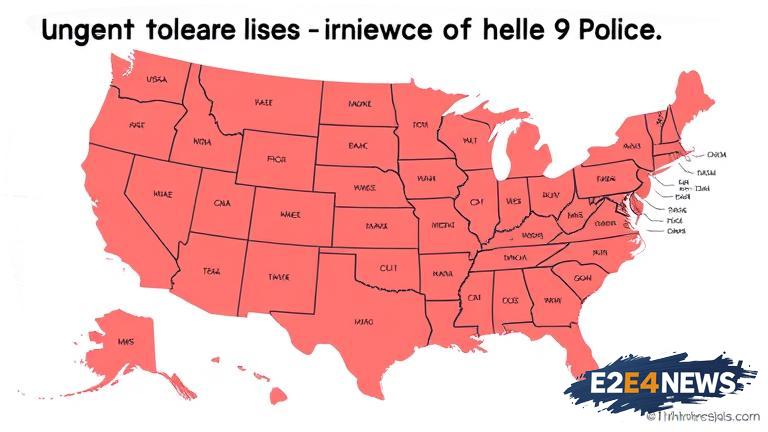
A recent study published in the field of hematology-oncology has shed light on the high prevalence of cross-state cancer care, where patients are seeking medical attention from healthcare providers in different states. This phenomenon has significant implications for the healthcare system, particularly in the context of telehealth. The study’s findings suggest that a substantial number of cancer patients are willing to travel across state lines to receive medical care, often due to a lack of specialized healthcare services in their home state. This trend is not only limited to patients with rare or complex cancers but also extends to those with more common types of cancer. The high prevalence of cross-state cancer care underscores the need for a comprehensive telehealth policy that can facilitate seamless communication and collaboration between healthcare providers across state lines. Telehealth has the potential to bridge the gap in healthcare access, especially for patients living in rural or underserved areas. However, the lack of a clear telehealth policy framework hinders the widespread adoption of telehealth services, ultimately affecting patient outcomes. The study’s authors emphasize that the development of telehealth policy is crucial to address the growing demand for cross-state cancer care. They suggest that policymakers should prioritize the creation of a telehealth infrastructure that can support the exchange of medical information, facilitate virtual consultations, and ensure continuity of care. Furthermore, the study highlights the importance of addressing the regulatory barriers that currently restrict the practice of telehealth across state lines. The licensure and reimbursement issues that plague telehealth services must be resolved to ensure that patients have access to high-quality care, regardless of their geographical location. The high prevalence of cross-state cancer care also raises concerns about the quality of care and patient safety. The study’s findings suggest that patients who receive care from out-of-state providers may experience delays in diagnosis and treatment, which can negatively impact their outcomes. To mitigate these risks, the development of telehealth policy must prioritize patient-centered care, ensuring that patients have access to timely and effective treatment. The study’s authors also emphasize the need for greater awareness and education about the benefits and limitations of telehealth services. Patients, healthcare providers, and policymakers must be informed about the potential of telehealth to improve patient outcomes and reduce healthcare disparities. In conclusion, the high prevalence of cross-state cancer care highlights the urgent need for telehealth policy that can address the complex issues surrounding healthcare access, quality, and patient safety. The development of a comprehensive telehealth policy framework is crucial to ensure that patients have access to high-quality, patient-centered care, regardless of their geographical location. As the healthcare landscape continues to evolve, it is essential that policymakers prioritize the creation of a telehealth infrastructure that can support the growing demand for cross-state cancer care. By doing so, we can improve patient outcomes, reduce healthcare disparities, and ensure that all patients have access to the care they need to thrive. The study’s findings have significant implications for healthcare providers, policymakers, and patients, emphasizing the need for a collaborative approach to address the challenges and opportunities presented by telehealth. Ultimately, the development of telehealth policy is critical to ensuring that patients receive high-quality, patient-centered care, and it is essential that we prioritize this effort to improve healthcare outcomes and save lives.